Infections and antibiotic resistance
Infections that our bodies are good at fighting off on their own, like coughs, colds, sore throats and flu, should be treated without antibiotics most of the time - just get plenty of rest and keep well hydrated.
Antibiotics are needed for bacterial infections, some of which may be potentially serious, e.g. sepsis, pneumonia, urinary tract infections, and meningococcal meningitis. So it is important that we use antibiotics only when necessary because using them when not needed, can lead to antibiotic resistance.
Antibiotic (or antimicrobial) resistance
Unfortunately, the overuse of antibiotics in recent years has meant they are becoming less effective. This has led to the emergence of antimicrobial resistance (AMR), which is when the bugs that cause disease are no longer affected by antimicrobial medicines such as antibiotics, that we use to treat them. This has led to the rise of superbugs. These are strains of bacteria that have developed resistance to many different types of antibiotics. Antibiotic resistance is made worse by:
- inappropriate use of available antibiotic medicines
- poor infection prevention and control
- a lack of medicines being developed to tackle emerging 'superbugs'
- insufficient global surveillance of infection rates.
It is important we tackle antibiotic resistance
We rely on antimicrobials such as antibiotics, antifungals, and anti-parasitic medicines, to treat the bugs that cause many common diseases. These bugs, however have already developed resistance to many antimicrobial medicines. There are few replacement antimicrobials in development and even fewer that target super resistant bugs.
As more bugs become resistant, more people will suffer for longer as infections become more difficult to treat - resulting in longer hospital admissions, routine surgical procedures becoming more dangerous to perform, and higher death rates.
Read more about antimicrobial resistance (AMR) and what the NHS is doing to try to address it. You can also watch the short video below developed by the UK Health Security Agency that explains a little more about antimicrobial resistance.
Information for parents and carers
Why a GP might not prescribe your child antibiotics, or write a
back-up (delayed) prescription.
In many cases, antibiotics do not usually speed up recovery, especially if the condition is caused by a virus. A GP might give you a delayed prescription for your child (usually 24-48 hours), if there is uncertainty whether your child will get better by themselves. It means you can keep a watch on your child's condition and if they do not get better, you will not have to make another appointment to get the antibiotics, but it also means that if their health improves, you will not have needed to give them the antibiotics unnecessarily. If your child continues to get worse after taking the prescribed antibiotics, you should seek further medical advice.
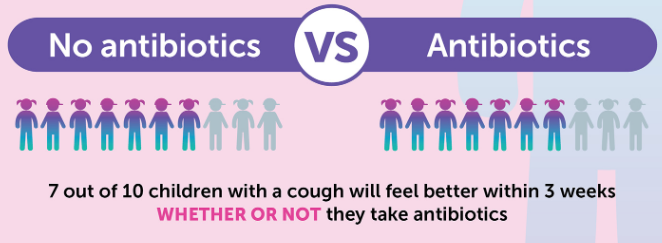
The below image shows the average recovery time for children who have had a cough and cold, both with and without antibiotics.
Do antibiotics have side-effects?
Yes, antibiotics can cause some side effects. The most common are diarrhoea and feeling sick. These are usually mild and should pass once the course of treatment has finished.
Rarely, some people may have an allergic reaction to antibiotics, especially penicillin and cephalosporins. In most cases, the allergic reaction is mild to moderate and can take the form of:
- a raised itchy skin rash
- coughing
- wheezing
- tightness of the throat, which can cause breathing difficulties.
These mild to moderate allergic reactions can usually be successfully treated by taking antihistamines. But if you're concerned, or your symptoms do not get better with treatment, call your GP for advice. If you cannot contact your GP, call NHS 111.
Severe allergic reactions
In rare cases, an antibiotic can cause a severe and potentially life-threatening allergic reaction known as anaphylaxis.
Call 999 or go to A&E now if:
- you have a skin rash that may include itchy, red, swollen, blistered or peeling skin
- you're wheezing
- you have tightness in your chest or throat
- you have trouble breathing or talking
- your mouth, face, lips, tongue or throat start swelling
You could be having a serious allergic reaction and may need immediate treatment in hospital.
What you can do to play your part in helping to reduce antibiotic resistance.
- Reduce the spread of germs by washing your hands regularly
- Always take antibiotics as prescribed and finish the full course
- Never take antibiotics prescribed to someone else or share yours with others
- If there are leftover antibiotics once the course is complete, take them to a pharmacy for safe disposal. Never flush them down the toilet or throw them in the bin. Do not keep them to use in the future.
For more information
World Health Organization Antimicrobial resistance
NHS Antibiotic resistance - NHS
UK HSA What is Antimicrobial Resistance (AMR) and how can you help combat it? – UK Health Security Agency

